Sutures and the problem of ‘stitch tunnels’
A particular problem with sutures used to close a circumcision wound is the formation of unsightly stitch tunnels. These are like tiny piercings that never go away. They can form around any suture material, but are more likely if absorbable material has been used externally. What happens is that the natural healing process forms a tunnel around the stitch. Thus the sutures should be removed as soon as the wound is strong enough to be self-supporting.
Sutures should be removed typically on the 7th or 8th day after circumcision; this is a simple process that can be carried out by a teenage or adult patient or the parent of a younger boy. A return to clinic or hospital should not normally be necessary unless the patient or parent is averse to carrying out this minor procedure. Self-removal has the advantage of being less ticklish; this is true of the removal of sutures from any scar - not just a circumcision scar.
Sutures should be removed typically on the 7th or 8th day after circumcision; this is a simple process that can be carried out by a teenage or adult patient or the parent of a younger boy. A return to clinic or hospital should not normally be necessary unless the patient or parent is averse to carrying out this minor procedure. Self-removal has the advantage of being less ticklish; this is true of the removal of sutures from any scar - not just a circumcision scar.
Materials from which suture thread is made
Non-absorbable sutures can be made from synthetic material (such as nylon or polypropylene, both of which are inert), silk (an animal protein) or cotton (a plant material). Non-dissolving sutures are usually coloured blue or black to make them more visible against the blood red of a wound. They normally have a smooth surface that allows them to be withdrawn easily.
Self-dissolving sutures can be made of:
Either type of suture - absorbable or non-absorbable - can be either monofilament or braided:
Suture strength:
The physical strength of any given suture material is designated by a standardised numbering system that takes into account both breaking strain and diameter. The degree of wound support achieved depends on this mechanical strength, on the number of stitches inserted and upon the adequacy of the anchoring of each one.
Because each suture becomes, from the point of view of the immune system, a “foreign body” and is also an additional wound, it is wise to use only what is necessary and no more. Excessive suturing is to be discouraged.
Self-dissolving sutures can be made of:
- Catgut (obsolete technology): A natural fibre made from the submucosa of the bovine intestine. It excites considerable inflammatory reaction and tends to potenciate infections. It loses strength rapidly and is of little use in modern surgery. Plain catgut dissolves more quickly than the type treated with chromium salts. Mentioned here for historic interest only.
- Vicryl /Dexon (Polyglactin): Dissolves more slowly than catgut but causes less of a reaction on implantation. Normally used only below the surface of the skin, it can also be used in areas where suture removal might jeopardize the repair such as with small children who might not cooperate with suture removal.
- Vicryl Rapide: A similar substance to Vicryl, but absorbed in a shorter period (5 days).
- Monocryl: The least reactive substance of this group and therefore the one that should leave least scarring. Unfortunately this is not a very soft material; it may be slightly irritating while the stitches are in place.
Either type of suture - absorbable or non-absorbable - can be either monofilament or braided:
Monofilament sutures cause less reaction than do braided sutures but require more ties to ensure an adequate maintenance of the knot compared to braided suture.
Braided sutures usually incite a greater inflammatory response but require fewer ties to maintain the knot’s integrity. Examples include silk, cotton and Mersilene.
Suture strength:
The physical strength of any given suture material is designated by a standardised numbering system that takes into account both breaking strain and diameter. The degree of wound support achieved depends on this mechanical strength, on the number of stitches inserted and upon the adequacy of the anchoring of each one.
Because each suture becomes, from the point of view of the immune system, a “foreign body” and is also an additional wound, it is wise to use only what is necessary and no more. Excessive suturing is to be discouraged.
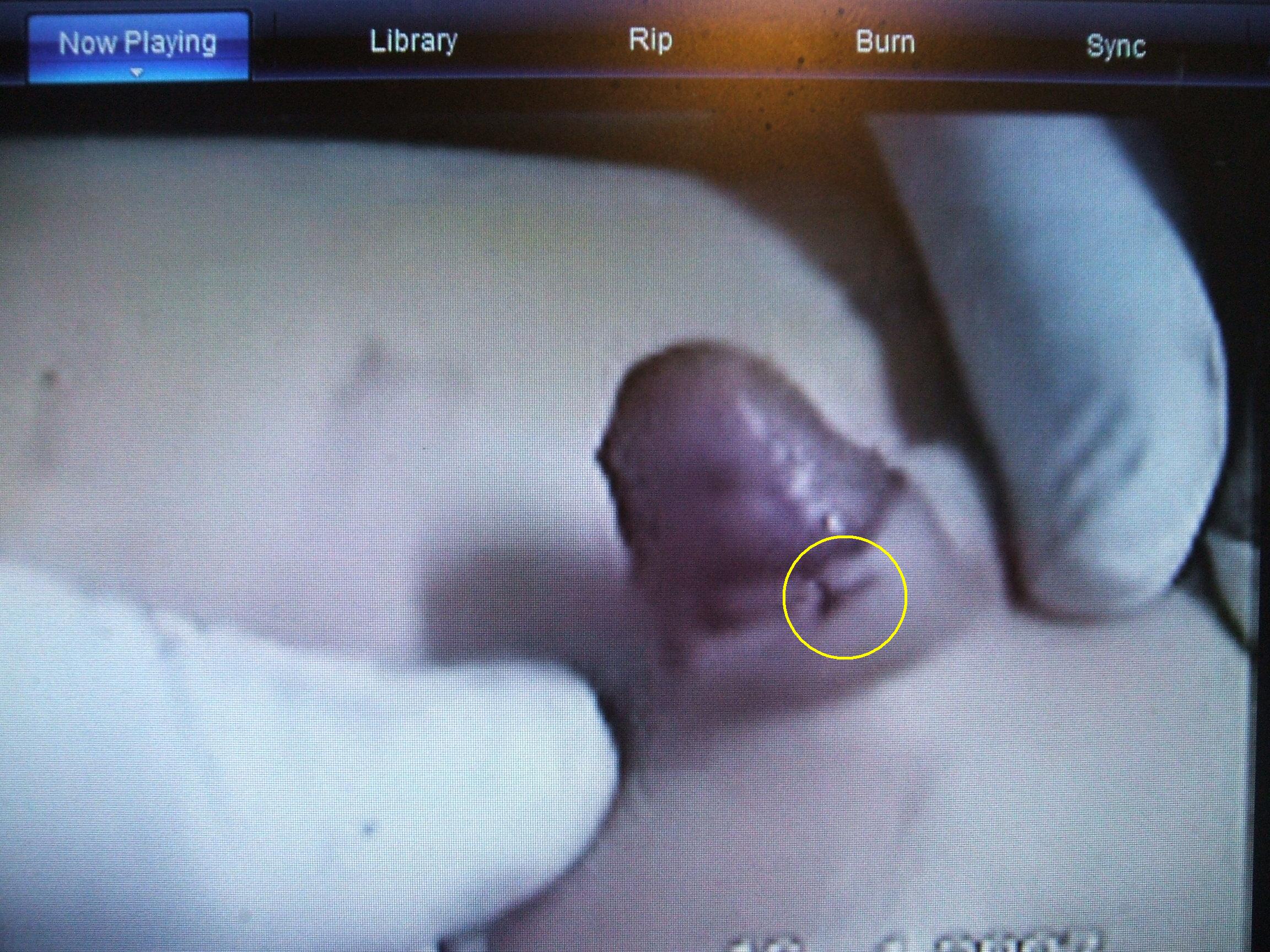
Patterns of suturing - the "T-shape" anchor:
In situations where a strong pull is likely to be applied to a stitch, it is important to anchor the stitch well so that it does not tear the tissue into which it has been inserted. This is normally achieved using a T-shaped stitch as illustrated in the following photographs. If an erection causes severe pulling, the "T" stretches into a "Y" shape. This compresses the tissue into which the energy is dissipated, doing so far more effectively than would be the case if the tension was applied directly to a single point of attachment. This makes a tear much less likely. The technique is particularly applicable to tight circumcisions, removal of shaft skin having left the erectile tissue with less opportunity for expansion than was the case previously. The pre-pubescent patient in the left-hand image below received 4 such sutures. The adult on the right received 16, on account of the greater tension that any erection of his would place on the healing scar.
| SUTURING TECHNIQUE FOR TIGHT CIRCUMCISIONS. | |
 |
 |
| © 2007 Professor Gamal Mousa Pre-pubescent boy being circumcised Low and Tight (glans:shaft ratio 67:33 or 2:1). Only 4 anchor sutures were deemed necessary to constrain any erections occuring during healing. |
© 2009 CIRCLIST Archives Circlist Member circumcised High and Tight as an adult. Close inspection of the scar line reveals the former position of 16 anchor sutures used to constrain erections during healing. |
CIRCLIST Member experiences of suturing:
When I had my circumcision, my doctor recommended to bathe my penis in warm camomile tea for 15-20 minutes several times a day until all stitches have dissolved and fallen off. I did so (using a toothbrush glass, by the way), and there are no stitch marks or even tunnels left. - Martin
--
Mine was done with soluble sutures, with no adverse effects. But the fact remains that non-dissolving ones are less likely to leave a mark, and less likely to get infected. I recently had a minor operation on my arm which was sutured with non-soluble ones and they were quite hassle-free and left no mark at all. (Actually my wife took them out - it doesn’t need a doctor to do it!)
In cosmetically sensitive areas such as faces non-dissolving sutures are always used. Why does the medical profession think that the penis is not cosmetically important? - Anonymous
--
Most of us circumcised as adults report having had dissolving (absorbable) stitches, which are obviously more convenient than ones which have to be removed. If my experience is any guide, removable ones may be less inclined to leave stitch marks. They are much finer and they can be removed as soon as they are no longer required (a week or thereabouts) whereas dissolving stitches may persist for considerably longer. My ‘second circumcision’ (properly called a revision) was performed by a plastic surgeon. It was a botch job, unsatisfactory enough to necessitate yet another revision; the result of mistakes on the part of several people. First, my GP for referring me to a plastic surgeon to do something right out his specialist field of competence. Second, me for not knowing better; I simple-mindedly thought that if anyone could do a neat cosmetic job, it would be a plastic surgeon. Third, and most culpable, the surgeon himself, for agreeing to perform a procedure he knew nothing about. But, getting back to the subject of stitches, he used silk stitches and - I have to admit - did a great job with them, leaving no stitch marks at all. - Anonymous
--
The stitch marks will never go away completely. The big problem with disolving stitches are skin tunnels, which are like piercings. They never go away either. My first circ left both tunnels and stitch marks. On my second circ and third partial circ, I had the stitches removed after a week and no mark or tunnel was left. The dotor told me just to let them dissolve, but I insisted that he remove them. The results were great. - Sam
--
The doctor did not cut my frenulum, so no sutures were required in that area.. There were 13 soluble sutures around my shaft, the last of which I removed on the10th day after the operation (May 19th 1978 to be precise!). Instinctively I knew they would cause scarring if left in too long, and I did get one small tunnel which has gone now.
If I have a regret it is that my scar is a thin white line, just a boundary between the two skin colours. I always wanted a nice brown ring, which I realize now is usually caused by the Gomco or TaraKLamps. I was circumcised freehand. - Anonymous
--
I had skin tunnels which lasted several years after I was circumcised (at age 20) even though I had non-dissolving stitches for the sutures. I finally treated it myself - I boiled a blade to sterilise it, swabbed my scar area with savlon, and for each tunnel, I inserted a needle down through the tunnel, and ran the blade down along shaft of the needle, quite safely removing the skin on top. It all healed nicely with the tunnels disappearing completely, though the stitch marks are quite visible. This alone, seems like a good argument to support routine infant circumcision. Have you ever seen a guy who was circumcised at birth that has skin tunnels? - Paul
--
Regarding self dissolving stitches; my surgeon who did my original circ put dissolving stitches in and told me to soak bandages off in a warm bath with some Savlon** in it. He said to take a daily bath and soak for a good 15 minutes, this caused the self dissolving stitches to keep soft and come out fairly quickly and leave no holes as some of you seem to have had. Perhaps you might like to try this and see if it helps.
**Savlon is a British personal disinfectant so you can use any brand common in your own country. Its use is basically to prevent the circumcision site getting infected. - Brian (UK)
--
Mine was done with soluble sutures, with no adverse effects. But the fact remains that non-dissolving ones are less likely to leave a mark, and less likely to get infected. I recently had a minor operation on my arm which was sutured with non-soluble ones and they were quite hassle-free and left no mark at all. (Actually my wife took them out - it doesn’t need a doctor to do it!)
In cosmetically sensitive areas such as faces non-dissolving sutures are always used. Why does the medical profession think that the penis is not cosmetically important? - Anonymous
--
Most of us circumcised as adults report having had dissolving (absorbable) stitches, which are obviously more convenient than ones which have to be removed. If my experience is any guide, removable ones may be less inclined to leave stitch marks. They are much finer and they can be removed as soon as they are no longer required (a week or thereabouts) whereas dissolving stitches may persist for considerably longer. My ‘second circumcision’ (properly called a revision) was performed by a plastic surgeon. It was a botch job, unsatisfactory enough to necessitate yet another revision; the result of mistakes on the part of several people. First, my GP for referring me to a plastic surgeon to do something right out his specialist field of competence. Second, me for not knowing better; I simple-mindedly thought that if anyone could do a neat cosmetic job, it would be a plastic surgeon. Third, and most culpable, the surgeon himself, for agreeing to perform a procedure he knew nothing about. But, getting back to the subject of stitches, he used silk stitches and - I have to admit - did a great job with them, leaving no stitch marks at all. - Anonymous
--
The stitch marks will never go away completely. The big problem with disolving stitches are skin tunnels, which are like piercings. They never go away either. My first circ left both tunnels and stitch marks. On my second circ and third partial circ, I had the stitches removed after a week and no mark or tunnel was left. The dotor told me just to let them dissolve, but I insisted that he remove them. The results were great. - Sam
--
The doctor did not cut my frenulum, so no sutures were required in that area.. There were 13 soluble sutures around my shaft, the last of which I removed on the10th day after the operation (May 19th 1978 to be precise!). Instinctively I knew they would cause scarring if left in too long, and I did get one small tunnel which has gone now.
If I have a regret it is that my scar is a thin white line, just a boundary between the two skin colours. I always wanted a nice brown ring, which I realize now is usually caused by the Gomco or TaraKLamps. I was circumcised freehand. - Anonymous
--
I had skin tunnels which lasted several years after I was circumcised (at age 20) even though I had non-dissolving stitches for the sutures. I finally treated it myself - I boiled a blade to sterilise it, swabbed my scar area with savlon, and for each tunnel, I inserted a needle down through the tunnel, and ran the blade down along shaft of the needle, quite safely removing the skin on top. It all healed nicely with the tunnels disappearing completely, though the stitch marks are quite visible. This alone, seems like a good argument to support routine infant circumcision. Have you ever seen a guy who was circumcised at birth that has skin tunnels? - Paul
--
Regarding self dissolving stitches; my surgeon who did my original circ put dissolving stitches in and told me to soak bandages off in a warm bath with some Savlon** in it. He said to take a daily bath and soak for a good 15 minutes, this caused the self dissolving stitches to keep soft and come out fairly quickly and leave no holes as some of you seem to have had. Perhaps you might like to try this and see if it helps.
**Savlon is a British personal disinfectant so you can use any brand common in your own country. Its use is basically to prevent the circumcision site getting infected. - Brian (UK)